Newly developed typhoid conjugate vaccines (TCVs) are safe, efficacious, and offer durable protection, making TCVs compatible with the Expanded Program on routine Immunization. Catch-up campaigns among children up to age 5 or 15 may also be appropriate in many settings. When deciding whether to implement TCV, cost-effectiveness is a critical consideration. In a recent article in The Lancet Infectious Diseases, authors Bilcke et al. provide strong evidence that TCV is likely to be cost-effective in most high- and medium-incidence Gavi, the Vaccine Alliance-eligible countries. This article supplements a paper by authors Lo et al., who reached a similar conclusion.
Now that we know that TCV is likely to be cost-effective in most medium- and high-burden settings, what should we do next? Of utmost importance, we need to strengthen efforts to ensure that TCV reaches the people that need it most. The World Health Organization has recommended TCV for use in all endemic countries, Gavi support is available for eligible countries, and the Typhoid Vaccine Acceleration Consortium (TyVAC) is implementing an integrated approach to accelerate scale-up of TCV.
While these important efforts continue, though, it’s not too early to start thinking ahead. As a scientific and public health community, we should start asking more nuanced questions―not “should we implement TCV?”, but rather “how, where, and how often should we perform catch-up campaigns, given local epidemiology and economic constraints?” We already know that TCVs are safe, effective, and will help prevent typhoid transmission. National decision-makers are considering whether to deliver catch-up campaigns at the national or sub-national level, whether to target all children under a certain age or specific age groups (e.g., those entering primary school), how to implement catch-up campaigns across a wide diversity of social and healthcare systems, and how frequently to perform catch-up vaccination in each setting.
These questions highlight the need to collect high-quality epidemiological data as TCV programs are implemented. For example, the studies above consistently show that TCV has the most impact and is most cost-effective in regions with a high burden of typhoid mortality. Yet, in most high-burden countries, surveillance systems are too weak to accurately estimate how many children die of typhoid. This needs to change. If we want to be able to deliver TCV to the children who need it most, we need to understand which children are at greatest risk. These data will also help us to more accurately estimate the number of lives saved from scaling up TCV, continue to build a more robust business case for data-informed TCV implementation, and hopefully, in the future, understand when TCV has done such an effective job of preventing typhoid such that catch-up campaigns are no longer necessary.
In summary, we now know that TCV is cost-effective―and the foremost priority needs to be effectively delivering this life-saving intervention to the children who need it most. But it is also time for the scientific and public health community to anticipate the next round of implementation questions that need to be answered, and for surveillance systems to be strengthened to better inform the typhoid response. Typhoid vaccines are already saving children’s lives―but as we continue to collect data and make strategic decisions, they can save many more.
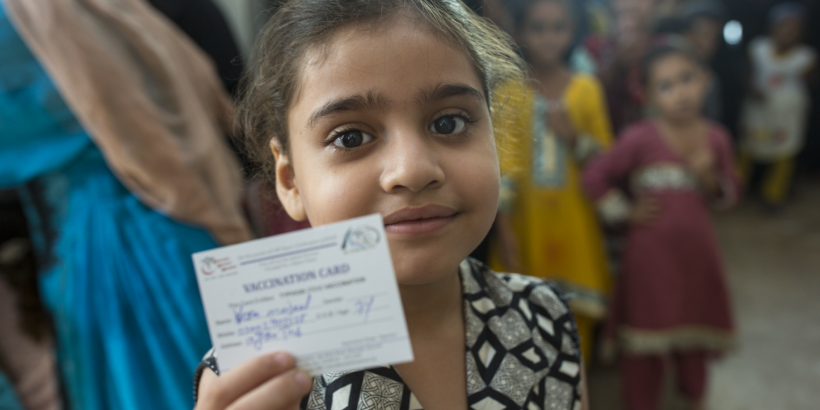
Photo: PATH/Asim Hafeez