Promises of magic bullet – or one-shot – solutions have a long history in public health, where interventions from water closets to antibiotics and vaccines were often touted as definitive interventions for a variety of diseases. However, rarely were these miracle solutions so straightforward. Our research on the history of typhoid in the UK, Ireland, and India shows how early public health practitioners and urban planners often neglected the complex biological and social drivers of disease prevalence in favour of single cure-all interventions. Wishful thinking also meant that solution templates developed for one part of the world were transposed onto other contexts without evaluating their suitability. The result were maladapted interventions that had little impact on disease transmission or created long-term problems of their own – many of which continue to have effects today.
Water and Sanitation
Access to clean water and effective sewerage are prerequisites for stopping the transmission of typhoid and other enteric diseases. However, varying climatic, hydrological, and social environments require different kinds of infrastructure. This lesson was often learned the hard way by those adopting sanitary systems developed for other geographic contexts.
From the 1850s onwards, major European and North American cities began to construct extensive water and sewage systems for their burgeoning populations as an effective preventative intervention for cholera (and later typhoid). Designed for temperate climates and inland urban spaces, Victorian sewage systems were based on the water-intensive collection, flushing, and dispersal of human faeces into rivers or coastal waters. Exporting these flush-based systems globally produced mixed results.
In British-ruled Ireland, Dublin planners decided to adopt a London-inspired system of intercepting sewers and a treatment plant for clarifying sewage in the 1870s. Following numerous delays, the so-called Main Drainage Scheme was opened in 1906 but Dubliners soon found that what worked for the fast-flowing Thames in London did not work in a shallow coastal estuary with tidal currents pushing sewage back onto foreshores and contaminating local shellfish banks with typhoid bacteria. Once in the ground, it proved difficult (and expensive) to rearrange the city’s sewage system. Contemporary changes to Dublin’s sewage system are still built on these Victorian foundations, and to this day, there are regular warnings about sewage pollution in Dublin Bay, and regular cases of gastrointestinal disease among swimmers.
In the city of Bangalore, India, a hauntingly similar problem was encountered in the mid-20th century when the city government attempted to build new “hygienic” suburbs. These new suburbs became hotbeds of typhoid when the recommended sewer systems overflowed in monsoon season, polluting wells and other water sources, and leading to the deaths of hundreds of new residents. The ambition of the project also outran its funding; once the half-built, defective sewers were in place, they remained so – and these neighbourhoods remain some of the highest-incidence areas of typhoid.
Diverting sewage to irrigate farmland also produced mixed results. Following the introduction of large-scale sewage farms in Berlin and Paris, engineers enthusiastically proposed similar plans for expanding cities in drier climates such as the US West or Mexico City and Santiago de Chile. Recycling raw sewage seemed an effective way of overcoming water limitations. However, planners did not pay sufficient attention to differences in cropping regimes. Following initial experiments with a range of plants including root vegetables, orchard fruits, and cabbage, municipal European and North American sewage farms mostly produced non-edible crops such as animal fodder, fibrous plants for the textile industry.[1] By contrast, local demand made producers in the Mezquital and Santiago de Chile favour market gardening and crops such as leafy vegetables. Spreading raw sewage over these crops easily spread typhoid. In Santiago de Chile, the local sewage farm was found to have caused a “hyperendemic” between 1970-1991 that undermined farms’ reputation as a water-saving intervention.
Vaccines
Problems of mal-adaptation and magic bullet thinking were not limited to infrastructure projects but extended to other forms of disease control ranging from behavioural to biomedical interventions such as mass-drug administration or vaccination.
Driven by advances in vaccine technology throughout the 20th century and the rise of cost-efficiency modelling, second and third-generation vaccines began to replace water-based interventions as a preferred form of international aid from the 1980s onwards. The success of vaccine-based interventions in rapidly developing middle-income countries such as China and Vietnam led many in the Global Health community to advocate for stand-alone vaccine campaigns as the primary response to both endemic and epidemic typhoid. What was, however, often forgotten was that historically successful vaccine control programs had been carried out amidst wider economic development and improvements of access to healthcare and safe water.
New generations of vaccines – including the latest generation of conjugate vaccines – are highly effective in curbing typhoid and protecting the most vulnerable. However, by themselves they will also not be a magic bullet. A growing proportion of the Global Health community therefore advocates that comprehensive typhoid control should rest on parallel investment in water, sanitation, and hygiene (WASH) infrastructure – especially with the spread of extensively drug resistant (XDR)-typhoid strains.
Think Global – Act Local
Abandoning the trope of the magic bullet in strategic planning remains challenging. As our brief historical overview shows, the last 150 years have seen significant advances in our ability to control the spread of typhoid and other enteric diseases. To be successful, every intervention – be it infrastructure or biomedical – needs to be adapted to local ecological and cultural contexts. This entails empowering local experts and decision-makers to develop a tailored and interlayered portfolio of interventions that they consider suitable and acceptable to local populations. In some cases, this will also entail rethinking elegant traditional intervention templates that do not satisfy local demands. Over reliance on single solutions carries significant risks – a lesson we cannot continue to repeat as we develop new typhoid control policies.
[1] Paris is a major exception where sewage was used to produce salad crops. European and North American authorities mandated non-edible plant production on raw sewage from the 1940s onwards.
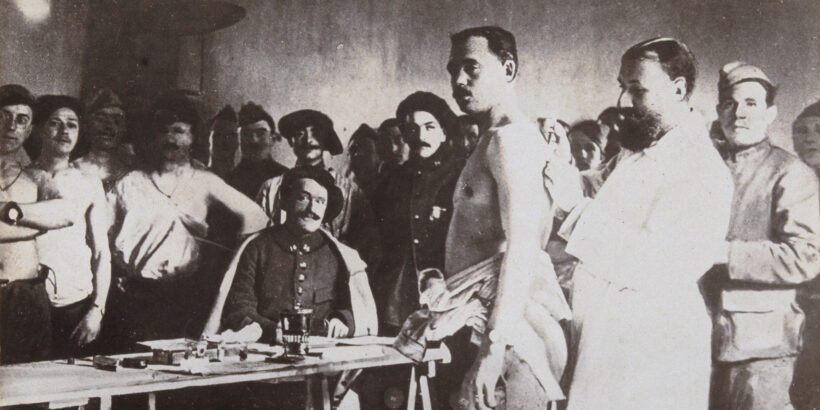
Cover Photo: Typhoid vaccination during world war one. Credit: Wellcome Collection.