Drug resistance, an urgent global health challenge in recent years, was described by the World Health Organization (WHO) in 2019 as “one of the top ten global threats to public health.” Also known as antimicrobial resistance (AMR), this occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to existing treatments such as antibiotics or antivirals.
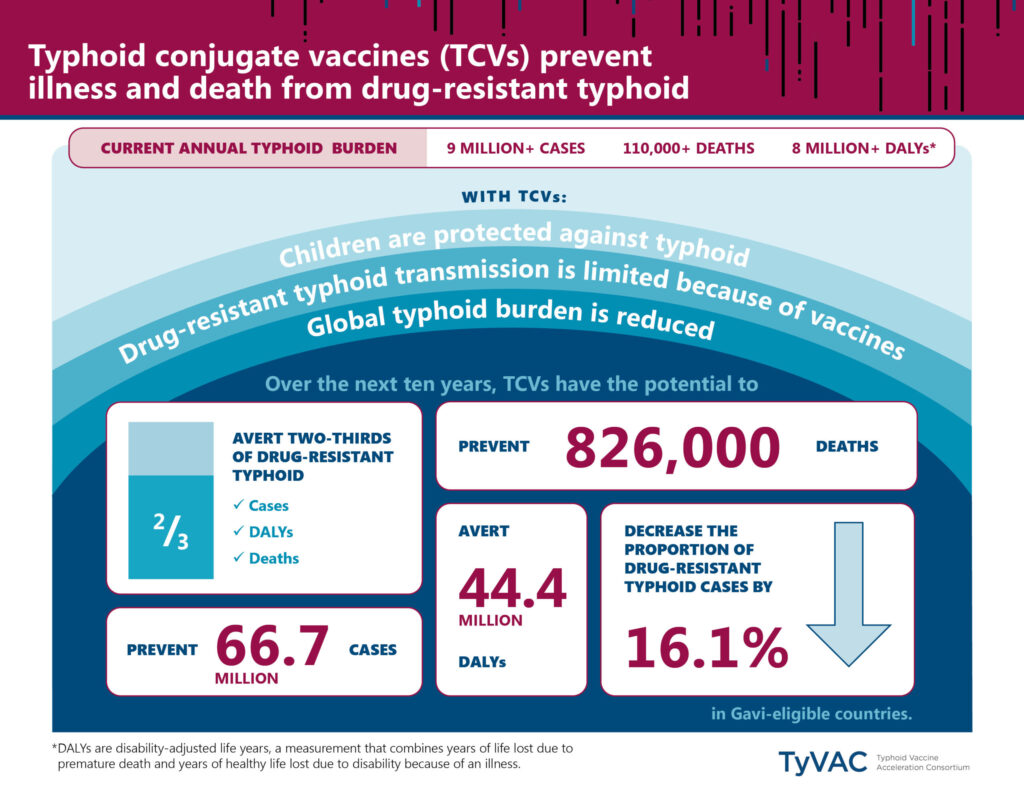
Recently released data from WHO, the International Vaccine Institute Korea, and the London School of Hygiene & Tropical Medicine highlight the need for increased urgency to prevent and control drug resistance. Data show that vaccines have the potential to avert half a million deaths associated with antimicrobial resistance annually. Analysis from the report included impact of new and existing global vaccines, including typhoid conjugate vaccines (TCV).
Drug resistant typhoid is a growing public health threat. Considering the recent study findings, we highlight five things everyone should know about drug resistant typhoid:
1) Drug resistant typhoid is worrisome trend
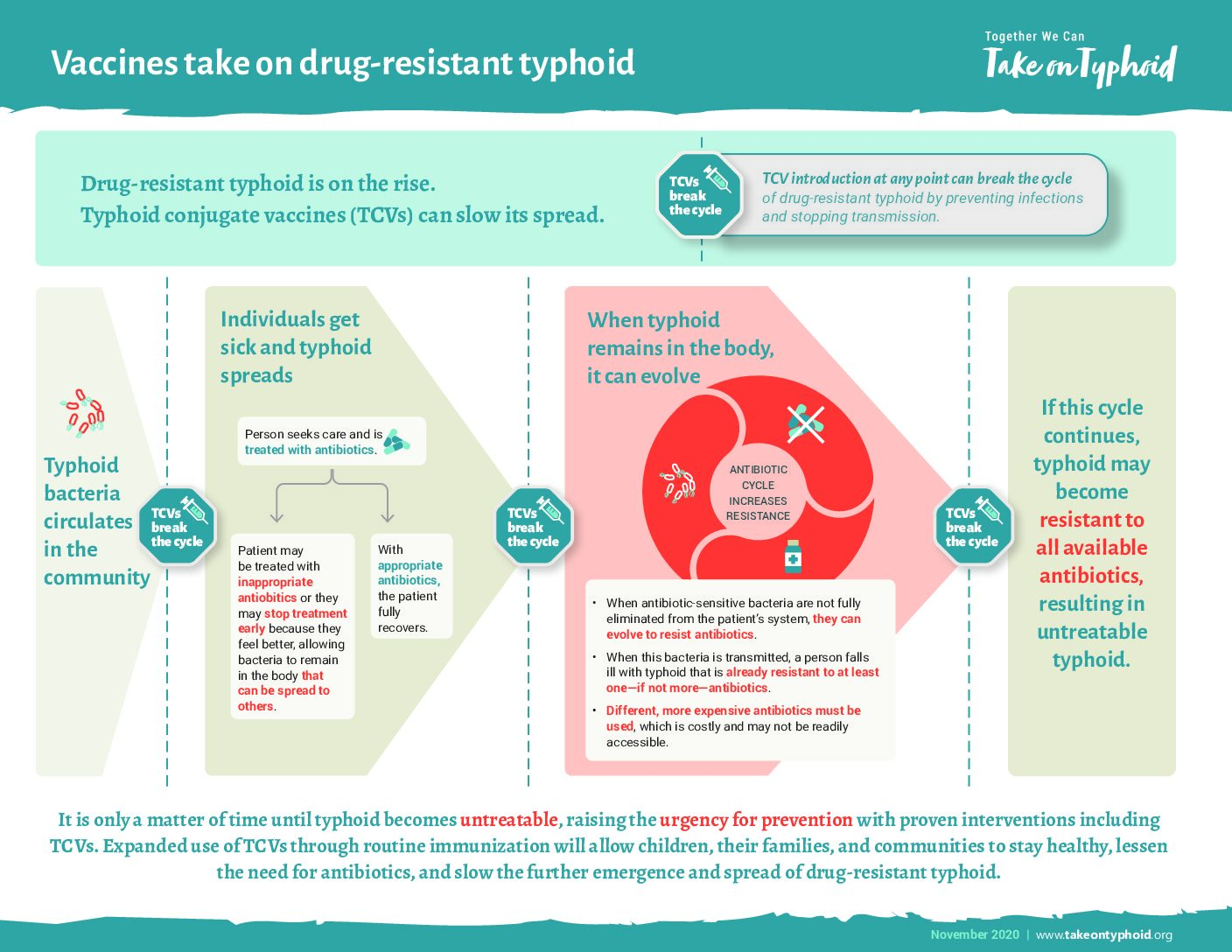
Drug resistant typhoid is a growing concern as the number of cases resistant to one or more antibiotics is increasing globally. Antibiotics, the only effective treatment for typhoid, have been used since the 1940s. However, since the 1970s, scientists have observed strains of typhoid bacteria that adapt to resist multiple classes of antibiotics. Identification of a drug resistant superbug, referred to as extensively drug resistant (XDR) typhoid, suggests that existing antibiotics may not effectively treat typhoid in the future. This raises the urgency for typhoid prevention before it becomes untreatable.
2) Drug resistance is a global problem
Drug resistant typhoid is a global threat as pathogens do not respect borders nor socioeconomic differences. As climate change and humanitarian disasters cause increased displacement of people, migration can lead to disease transmission. Transitory and migratory populations often live in conditions that lack safe water and improved sanitation and are therefore at increased risk of typhoid. As these populations move, particularly from rural to urban areas, pathogens travel with them, and can become a dire health problem for local health systems and communities.
To combat increasingly resistant pathogens, we need collective global action. WHO urges countries to develop national action plans against drug resistance, which should specifically include vaccines like TCV, as a priority intervention. Plans and actions at the national level connect regional and global progress so that we can take on typhoid together.
3) Low- and middle-income countries bear the burden of drug resistant typhoid
While drug-resistant typhoid is a challenge globally, low- and middle-income countries are most negatively impacted. Many low-income countries lack infrastructure for safe water, sanitation, and hygiene (WASH), which can increase risk of water-borne diseases like typhoid. Further, low-income countries are often most impacted by the effects of climate change, including extreme flooding and droughts, which similarly increases risk of typhoid. With increased risk of disease comes the potential for increased cases of drug resistant typhoid.
Limited laboratory capacity and inadequate surveillance have contributed to increased drug resistance within the world’s most vulnerable populations. With limited access to lab testing, presumptive or clinical diagnosis can lead to inappropriate use of antibiotics. This is most often seen in countries with poor health systems where accurate diagnosis and appropriate treatment are out of reach in the communities most at risk for typhoid.
4) Drug resistant typhoid is costly
Typhoid treatment is expensive, burdening families with treatment costs, transportation expenses, medical bills, and time lost from work due to illness or caring for a loved one. Data from Malawi show that 44% of households incur catastrophic costs when a family member has typhoid. These expenses increase for drug-resistant typhoid cases. Treatment of drug-resistant typhoid requires antibiotics that are more difficult to access and often more expensive to the patient and health care system. Drug resistant typhoid often requires a longer treatment period, therefore increasing expenses and prolonging time away from employment.
5) Typhoid conjugate vaccines help prevent and control drug resistance
TCVs protect against typhoid, including drug-resistant strains, in a single dose. This limits transmission and further evolution of drug resistant strains. Data show that TCVs can help to effectively control drug-resistant typhoid outbreaks as happened in Pakistan and Zimbabwe. Research from Pakistan found TCV to be 97% effective against XDR typhoid. According to the most recent WHO data, increased coverage of TCVs are an effective means to reduce drug resistant typhoid.
Although drug resistant typhoid is not new, we continue to identify drug resistance pathogens in new places which helps to track transmission patterns. Ongoing research and surveillance add to our understanding of drug resistance. We must work together to increase TCV introduction and access to improved WASH resources to reduce global typhoid burden and prevent the spread of drug resistant strains.