Typhoid, currently endemic in many parts of Asia and Africa, remains a major public health challenge. It can be effectively treated with antibiotics, but drug resistance is increasing. This makes typhoid more difficult to treat, forcing the use of more expensive and less available antibiotics. We spoke with Dr. Zoe Dyson about genome sequencing and a new data visualization tool to better understand the emergence and spread of drug-resistant typhoid and support decision-making for typhoid conjugate vaccine (TCV) introduction.
What is TyphiNET?
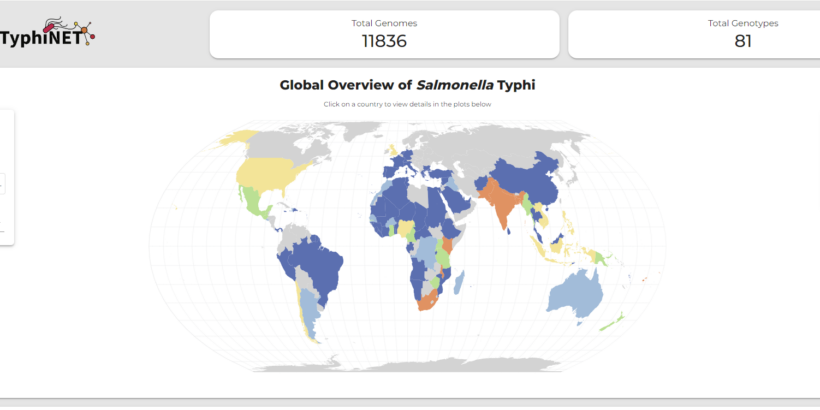
Dr. Dyson: TyphiNET is an interactive online dashboard that allows users to explore typhoid drug resistance data. One of the exciting things about it is that it provides country-level summaries on drug-resistant typhoid, from what strains are present in a country, to drug resistance trends for different antibiotic treatment options over time. The database contains nearly 12,000 typhoid genomes from 101 countries. Importantly, TyphiNET is populated by high-quality data curated by the Global Typhoid Genomics Consortium that is analyzed using the Pathogenwatch platform. The database will update as additional genomes are released.
Whole genome sequencing data are a rich source of information on typhoid variants, drug resistance prevalence, and mechanisms of how typhoid strains acquire resistance to antibiotics. An easy-to-use platform that combines available data in one place can help a variety of stakeholders, from clinicians who need to choose the right antibiotic for their patients, to policymakers making decisions on vaccine introduction and prevention strategies. This is what TyphiNET strives to do.
How can these data be used for country TCV introduction decision-making?
Dr. Dyson: The World Health Organization recommends TCV introduction in countries that have a high burden of typhoid and/or a high burden of drug-resistant typhoid. National-level drug-resistance data can help make the case for investment in national immunization programs. However, these data haven’t been consistently gathered, and typhoid drug-resistance data remains scarce in most typhoid-endemic countries. Where it is available, existing resources containing the data have been difficult to access, requiring users to have a background in genomics to interpret results. Additionally, the data have been spread out across multiple different databases instead of one central location.
With TyphiNET, decision-makers can filter and analyze available drug-resistance data from their country and/or region to better understand typhoid drug resistance trends and prevalence. This information can support country prioritization and decision-making for typhoid prevention and control strategies, including TCV introduction.
However, there are many typhoid endemic countries where we are lacking data, underscoring the need for greater investments in blood-culture infrastructure and environmental surveillance to better understand the prevalence of both circulating pathogen variants and resistance to clinically relevant drugs more widely. As genome data derived from these efforts emerge, TyphiNET will be routinely updated to provide up-to-date surveillance data.
How did you ensure that the tool is accessible to those without a genomics background?
Dr. Dyson: While developing the dashboard, we asked untrained users from different geographies to explore the site and answer 10 multiple choice questions designed to assess whether users could successfully navigate the dashboard to find answers to specific questions about prevalence trends, and determinants of typhoid resistance in specific countries and time periods. The results suggest that the dashboard is intuitive for users familiar with the concepts of drug resistance to find the correct answers to these types of questions. This gives us confidence that TyphiNET can increase access to this type of information for a broader user-base, including public health officials who may not have deep knowledge in genomics.
A manuscript further describing the tool, as well as case studies highlighting the utility of TyphiNET to understand national typhoid drug-resistance trends, is available for further reading.
Photo: The TyphiNET dashboard.